A Gentle Reminder to Make Time for Yourself
Those who work in the palliative care environment are exposed regularly to deep, existential issues, challenging psychological situations and heightened emotional distress. In this article, we’ll look at the basics of self-care and the building blocks of mindfulness, which anyone working within a palliative care system, whether at Calvary or another end-of-life care setting, should take to heart.
Nurture Self-Care

RN, MS, RN Administrator, Calvary Hospital – Brooklyn Campus
Self-care is a discipline. For trained caring professionals in the helping fields, your knowledge and practice of self-care is essential to your ability to foster a healing relationship with your patients.
Identifying practical activities that help you cope with frequent exposure to the challenges present in an end-of-life care setting can increase the quality of life enjoyed by both you and your patients.
“As a nurse for more than 30 years, I have discovered first-hand the value of self-care,” said Patricia M. Caffrey, RN, MS, RN Administrator, Calvary Hospital – Brooklyn Campus. “Your priority as a palliative care professional is to care for yourself regularly. That will maximize your ability to help your patients.”
The goal of self-care is to promote health, improve care and increase people-focused support resources and opportunities.
Take Inventory of Your Feelings
Like any skill performed in your professional life, self-care requires practice. However, changing personal behaviors and attitudes can be challenging. It’s easy to fall back into poor health habits when stress mounts. Start by conducting an inventory of your own feelings.
See if any of these questions apply to you:
- Do you have extreme fatigue after leaving a shift?
- Do you have trouble sleeping?
- Do you worry or feel anxious about current or past patients?
- Does your spouse or family remind you that there’s a life outside of work?
- Do you have difficulty mentally leaving behind the tragedies of the day?
- Do you often think back to choices you made during the day to see how they could have gone differently?
- Have you ever had difficulty empathizing with your patients and their families?
If you answered “yes” to any of these questions, you may be in need of self-care.
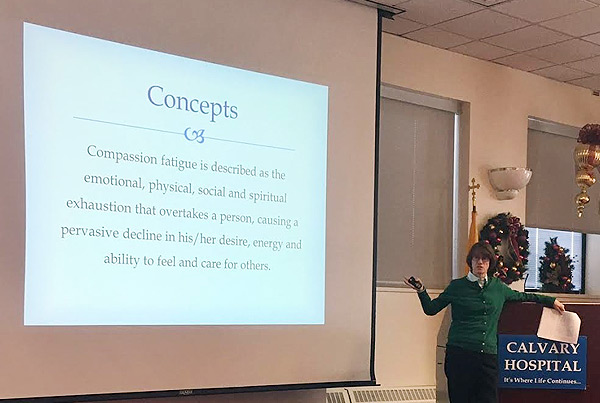
Do You Have Compassion Fatigue?
The emotional and spiritual stress of working in a palliative care environment often causes feelings of emotional exhaustion. Compassion fatigue is a common experience in people helping others in distress.
When a preoccupation with the suffering of those you care for builds, it can create a secondary traumatic stress and lead to bad outcomes. It causes great workers to leave their jobs or worse. It can turn into chronic fatigue, unhealthy lifestyle habits and depression.
If you think you may be suffering from compassion fatigue, you probably are! Fortunately, awareness of compassion fatigue symptoms can lead to positive change, personal growth and a renewed sense of resiliency.
Finding Balance
In end-of-life settings a lot is being asked of you as a professional. Your role is to connect with people and provide the best care possible. To be effective you must share love and show tremendous empathy.
However, you are human, and you need to have balance. You cannot and won’t always be “on.” Listen to your body and take time to do activities that restore you psychologically and emotionally. Create healthy habits that support your regular practice of these activities.
Develop Mindfulness
Over time the pressure of palliative care can begin to weigh on you, no matter how much you love your job or how deep your commitment to your patients. When you are stressed, self-care activities are usually the first thing you neglect, which is why mindfulness is critical to self-care.
Mindfulness can be defined as, “The basic human ability to be fully present, aware of where we are and what we’re doing, and not overly reactive or overwhelmed by what’s going on around us,” according to Mindful, a blog dedicated to a “healthy mind, healthy life.”
While everyone possesses the ability to enjoy the calm that mindfulness can bring, daily practice will help you reach this state more readily.
Establish a Self-Care Plan
You cannot pour from an empty cup. Strive to keep your body healthy to avoid or reduce the effects of secondary trauma. Find a healthy balance between your work-related stresses and everyday home life in order to prevent compassion fatigue.
Self-care can help you gain a deeper level of self-awareness in which you explore activities that bring joy, provide comfort and change a negative or harmful mindset.
Take a moment each day to:
- Acknowledge your reactions to difficult situations and allow yourself time to cope. Even if you only have 60 seconds, practice mindfulness, repeat an empowering or calming mantra, or learn the STOP stress reduction method developed by Elisha Goldstein Phd.
- Be aware of your own stress levels and take action before reaching your limits.
- Nurture mutually supportive relationships with others involved in palliative care. Make time to talk, sharing concerns but also happy experiences.
- Exercise, do yoga or meditate to keep your body strong and flexible.
- Get adequate sleep and eat foods that will nourish your body and mind.
By taking these initial steps, you’ll be on your way toward developing a self-care plan that will, in time and with practice, take root in your day-to-day habits. The work you do is important. Ensuring your mind and body are healthy supports your ability to provide the best possible care for your patients.
Categories
Archives
- April 2024
- March 2024
- February 2024
- December 2023
- November 2023
- October 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- January 2023
- December 2022
- October 2022
- August 2022
- July 2022
- June 2022
- April 2022
- March 2022
- February 2022
- January 2022
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- April 2012